Pancreatology Details

Pancreatology is a specialized branch of medicine that focuses on the study, diagnosis, and treatment of diseases affecting the pancreas. The pancreas is a vital organ located behind the stomach, playing a crucial role in digestion by producing enzymes and regulating blood sugar levels through insulin and other hormones. Pancreatologists are medical specialists with expertise in managing pancreatic disorders, which can range from acute conditions to chronic diseases. Key areas within pancreatology include:
Acute Pancreatitis: A sudden inflammation of the pancreas that can cause severe abdominal pain, nausea, and vomiting. Acute pancreatitis is often linked to gallstones, excessive alcohol consumption, or certain medications. It may require hospitalization and supportive care.
Chronic Pancreatitis: Long-term inflammation that leads to permanent damage to the pancreas, impairing its ability to produce digestive enzymes and hormones like insulin. This condition can result from prolonged alcohol abuse, genetic factors, or autoimmune conditions and often leads to malnutrition and diabetes.
Pancreatic Cancer: Pancreatic cancer, particularly pancreatic ductal adenocarcinoma, is one of the most aggressive and deadly cancers. Early symptoms are often vague, such as abdominal pain, weight loss, and jaundice, making early diagnosis challenging. Treatment may involve surgery, chemotherapy, radiation, or targeted therapies.
Pancreatic Cysts: Fluid-filled sacs within the pancreas, which can be benign or potentially precancerous. Some cysts, like intraductal papillary mucinous neoplasms (IPMNs), can increase the risk of developing pancreatic cancer and may require monitoring or surgical removal.
Pancreatic Insufficiency: A condition where the pancreas doesn't produce enough digestive enzymes, leading to malabsorption of nutrients, weight loss, and gastrointestinal issues like diarrhea or fatty stools (steatorrhea). This is often associated with chronic pancreatitis or cystic fibrosis.
Diabetes Mellitus: Although primarily an endocrine condition, pancreatologists are involved in managing diabetes when it results from pancreatic diseases. Type 1 diabetes can occur when autoimmune destruction affects the insulin-producing cells in the pancreas, while Type 2 diabetes may develop due to insulin resistance.
Cystic Fibrosis-related Pancreatic Disorders: Cystic fibrosis can cause the pancreas to produce thick, sticky mucus that blocks enzyme release, leading to malnutrition and digestive problems. Pancreatologists manage the complications arising from this genetic condition.
Pancreatic Trauma or Surgery: In cases of pancreatic injury due to accidents or as part of complex surgeries (such as the Whipple procedure for pancreatic cancer), pancreatologists work with surgical teams to manage postoperative care and complications.
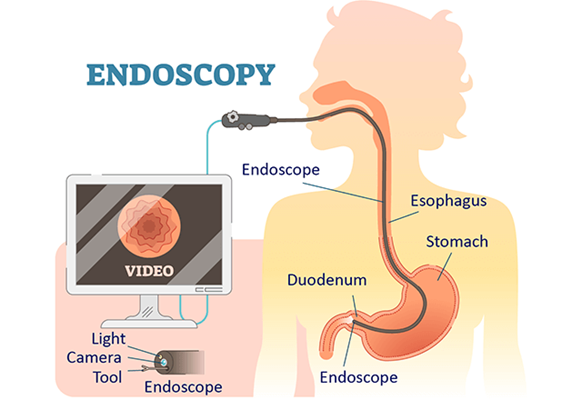
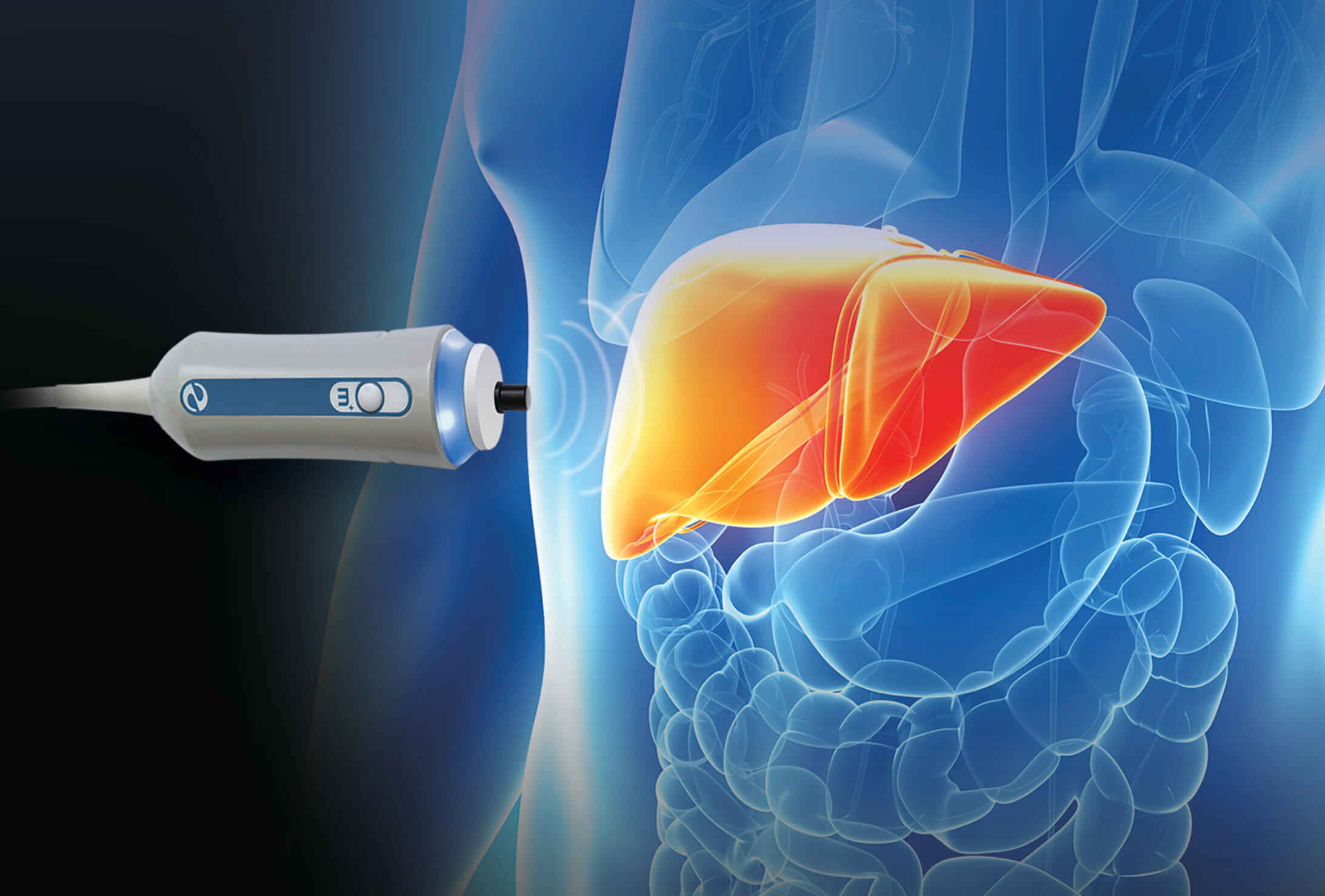
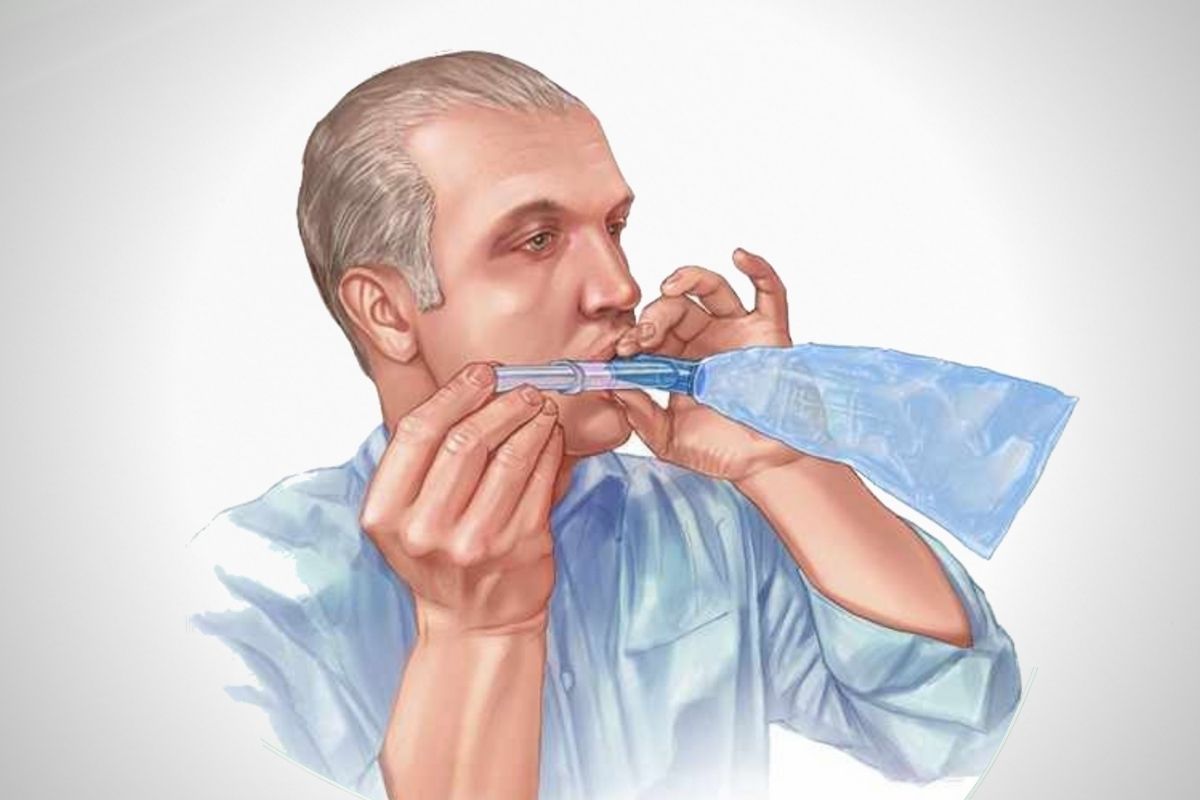
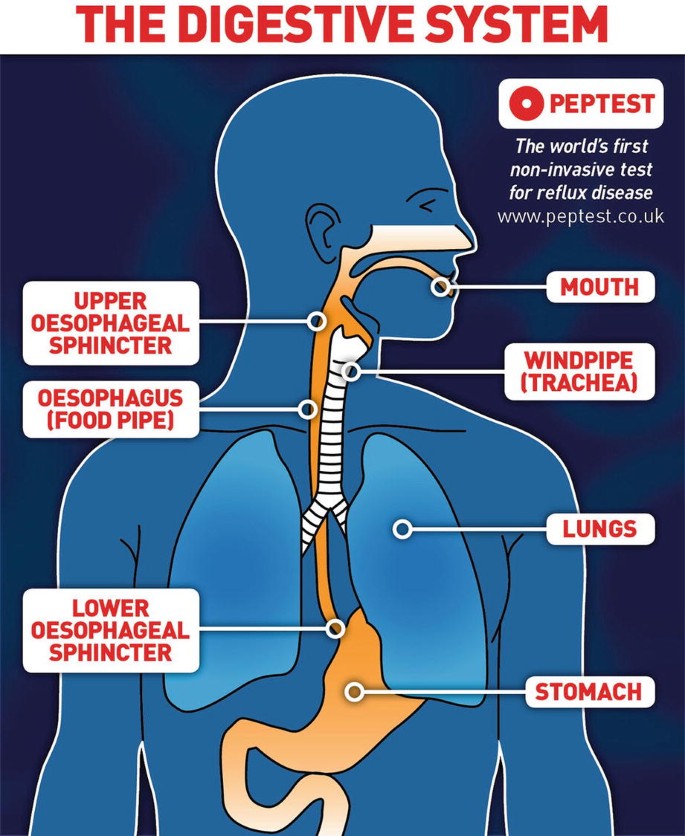
Pancreatologists often work with diagnostic techniques such as endoscopic ultrasound (EUS), magnetic resonance cholangiopancreatography (MRCP), and CT scans to assess pancreatic structure and function. Treatment options depend on the specific condition and may range from enzyme replacement therapy and lifestyle modifications to more invasive procedures like surgery or endoscopic interventions.